Pulmonary Fibrosis
Pulmonary fibrosis (PF) is a form of interstitial lung disease that causes scarring in the lungs. There are over 200 different types of PF and in most cases, there is no known cause. Four categories of PF are:
- Idiopathic Pulmonary Fibrosis (IPF) - The most common type pulmonary fibrosis. Idiopathic means that cause is unknown. Most IPF patients start noticing symptoms between the ages of 50 and 70 years old.
- Disease - Some autoimmune diseases like rheumatoid arthritis, scleroderma or Sjogren's syndrome can cause scarring in the lungs. People with viral infections and gastroesophageal reflux disease (GERD) are also risk factors for PF.
- Familial - This type is very rare. PF is considered familial when two or more members within the same family have idiopathic pulmonary fibrosis.
- Exposures - PF can be caused by exposure to hazardous materials. Examples include occupational exposures such as asbestos or silica. Some cases of PF are caused by breathing in bird or animal droppings. Radiation treatments and certain types of medications can cause PF. Cigarette smoking also increases the risk of developing PF.
Symptoms
One reason pulmonary fibrosis often goes misdiagnosed is that symptoms of PF can be similar to symptoms of other lung diseases. Symptoms include:
- Shortness of breath particularly during exercise
- Dry, hacking cough
- Fast, shallow breathing
- Gradual unintended weight loss
- Tiredness
- Aching joints and muscles
- Clubbing (widening and rounding) of the tips of the fingers or toes
Diagnosis
The first step to diagnosis pulmonary fibrosis is to review symptoms, collect family history
of lung disease, any exposure to hazardous materials, and any past disease treatments. A physical exam will be performed to include listening for crackling sounds in lungs.
A battery of tests will be performed including:
- Pulmonary function test
- Six-minute walk test
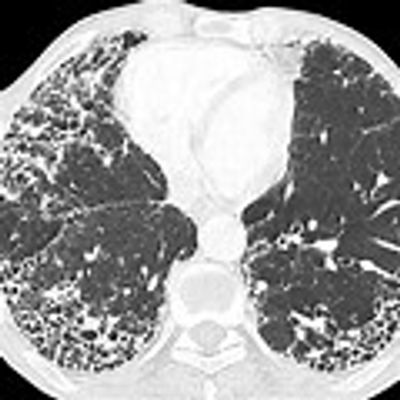
- High-resolution CT scan
Treatment
If you are diagnosed with PF, it is important to know how to take care of yourself, eating right and exercise. No one can predict your experience. Some treatment options to expect after a PF diagnosis are:
- Supplemental oxygen
- Medication
- Pulmonary rehabilitation
- Lung transplant
- Good support system.
Hypersensitivity Pneumonitis

Hypersensitivity pneumonitis is caused when you breathe in a specific substance (allergen) that triggers an allergic reaction in your body. These allergens are often naturally occurring—such as bird feathers or droppings, household mold and animal dander.
Sometimes hypersensitivity pneumonitis can cause permanent lung scarring if it is not detected early and you continue to be exposed to the allergen.
Common allergens have been given specific names that relate to the problem including:
- Farmer's lung - breathing in mold that grows on hay, straw and grain
- Bird fancier's Lung - breathing particles from feathers or droppings of many species of birds.
- Humidifier lung - breathing fungus growing in humidifiers, air conditioners and heating systems.
- Hot tub lung - breathing in bacteria that may be found in the water vapor for indoor hot tubs.
Symptoms
Acute Attack
- Flu like symptoms
- Fever
- Chills
- Muscle aches
- Headache
- Cough
Chronic Hypersensitivity Pneumonitis
- Shortness of breath
- Tiredness
- Cough lasting for weeks
- Weigh loss
Diagnosis
Diagnostic tests to confirm hypersensitivity pneumonitis include:
- Chest X-ray and CT Scan
- Pulmonary function test
- Blood tests
- Bronchoscopy
- Surgical lung biopsy
Management and Treatment
The first step of managing hypersensitivity pneumonitis is to take appropriate measures to avoid or eliminate the allergen from your home or workplace If caught early, staying away from the source can help reverse the damage and after a short time, the lungs will return to normal.
In more severe cases, avoidance may not be enough. Treatment may include corticosteroids or other immunosuppressive medication to reduce inflammation and prevent your immune system from reacting to the allergens you inhale.
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.